Back surgery (spinal surgery)
Treatment to relieve pain from compressed nerves in your spine.
At Spire our highly skilled surgeons and expert aftercare team use trusted and clinical proven surgical techniques to repair damage to your back and help you enjoy your usual activities again.
Sometimes also called
- Discectomy
- Laminectomy
- Lumbar decompression
- Microdiscectomy
- Spinal decompression surgery
- Spinal fusion test
At a glance
-
Typical hospital stay
1-4 days -
Procedure duration
At least an hour, varies according to type of surgery -
Type of anaesthetic
General -
Available to self-pay?
Yes -
Covered by health insurance?
Yes
Why Spire?
- Fast access to treatment when you need it
- Consultants who are experts in their field
- Clear pricing with no hidden charges
- 98% of our patients are likely to recommend us to their family and friends
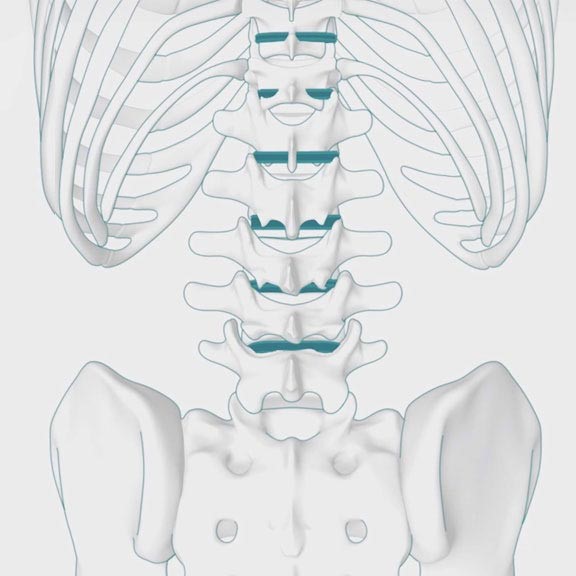
Your spine is made up of bones called vertebrae, which are cushioned by discs of tissue that act as shock absorbers. Your spinal cord runs through a channel in the spine and it is here that nerves branch off to the rest of the body. When one or more nerves in your spine are put under pressure they can cause pain, and back surgery may be performed to relieve some of this pressure.
Why you might need it
Pressure on the spinal nerves causes problems with the traffic of nerve signals to and from the brain. Compressed nerves can also lead to sciatica, which is usually seen with these symptoms:
- pain in the lower back, buttock, leg and foot
- pins and needles
- muscle weakness and/or wasting
- loss of sensation
The type of surgery recommended for you will depend on the source of your back pain, as there are several causes of nerve compression. These include:
- Disc prolapse/herniation – More commonly known as a 'slipped' disc, this occurs when a disc of tissue bulges out between two vertebrae
- Spinal stenosis – This happens when the spinal canal becomes narrow due to cartilage in the vertebrae becoming worn or inflamed
- Spondylolisthesis – This is the name for when a vertebrae slips out of position
We pride ourselves on our clinical excellence, you'll be looked after by an experienced multidisciplinary care team.
Find a Spire hospital offering this treatment

Who will do it?
Our patients are at the heart of what we do and we want you to be in control of your care. To us, that means you can choose the consultant you want to see, and when you want. They'll be with you every step of the way.
All of our consultants are of the highest calibre and benefit from working in our modern, well-equipped hospitals.
Our consultants have high standards to meet, often holding specialist NHS posts and delivering expertise in complex sub-specialty surgeries. Many of our consultants have international reputations for their research in their specialised field.
Before your treatment
You will have a formal consultation with a healthcare professional. During this time you will be able to explain your medical history, symptoms and raise any concerns that you might have.
We will also discuss with you whether any further diagnostic tests, such as scans or blood tests, are needed. Any additional costs will be discussed before further tests are carried out.
Preparing for your treatment
We've tried to make your experience with us as easy and relaxed as possible.
For more information on visiting hours, our food, what to pack if you're staying with us, parking and all those other important practicalities, please visit our patient information pages.
Our dedicated team will also give you tailored advice to follow in the run up to your visit.
If you normally take medication (eg tablets for blood pressure), continue to take this as usual, unless your surgeon or anaesthetist, specifically tells you not to. If you're unsure about taking your medication, please contact the hospital.
The procedure
We understand that having surgery can potentially be a time of anxiety and worry. Our experienced and caring medical staff will be there for you, holding your hand, every step of the way.
Back operations are generally done under general anaesthetic, which means you are asleep throughout the procedure and feel no pain. The operation may be done by open surgery, which involves a large cut being made in your back, or keyhole surgery, which uses a thin and long microscope and other special instruments through several small incisions on your back. Your surgeon will discuss with you which type of back operation is most suitable for your pain.
Common treatments include:
Discectomy or microdiscectomy
This procedure, the centre of the disc that is affecting the spinal cord or nerve is removed; this relieves the pressure and the pain caused by the protruding disc.
Nerve root or spinal decompression
The nerve root or spinal decompression method is done to remove any bone, disc tissue or other material that is putting pressure on the nerve or spinal cord areas.
Spinal fusion
Vertebrae are joined together using bone taken from your hip, metal implants or a specially designed cage.
Your surgeon may perform more than one type of procedure, if needed, during a single operation.
Aftercare
Depending on the type of operation you have, you will usually need to stay in hospital for between two and seven days.
After the procedure, you will be taken from the operating theatre to a recovery room, where you will come round from the anaesthesia under close supervision.
After this, you will be taken to your room where you can rest and recuperate until we feel you’re ready to go home.
While you are in hospital a physiotherapist will help you exercise while you are in bed and then will be able to help you get up and down the stairs before you are discharged.
Pain relief
Your anaesthetist will prescribe painkillers after the operation. Suffering from pain could slow down your recovery, so please discuss any discomfort with your doctors or nurses.
We will provide you with a supply of all the medicines your consultant feels you need to take home with you after you've left hospital, up to 14 days. This may be at an additional cost to some patients.
Recovery time
You should gradually increase the amount of walking and sitting you do during the first month after your surgery. During this time you should avoid bending, lifting, twisting or stretching. Your surgeon will give advice that is specific to you about how soon you can return to work and leisure activities such as sport.
How your loved ones can help
Once you’re ready to be discharged from hospital, you’ll need to arrange a taxi, friend or family member to take you home as you won’t be able to drive. You need to follow your surgeon’s advice about driving. You shouldn’t drive until you are confident that you could perform an emergency stop without discomfort.
Looking after you
Even after you’ve left hospital, we’re still looking after you every step of the way.
Typically your consultant will want to see you after your treatment to see how you’re doing. You might also be seen by one of our physiotherapists.
On rare occasions, complications following back surgery can occur. If you experience any of these symptoms – infection, excessive bleeding, blood clots, numbness, loss of muscle control, pain or paralysis – call us straight away.
The chance of complications depends on the exact type of operation you are having and other factors such as your general health. We will talk to you about the possible risks and complications of having this procedure and how they apply to you.
If you have any questions or concerns, we’re ready to help.
Why choose Spire?
We are committed to delivering excellent individual care and customer service across our network of hospitals, clinics and specialist care centres around the UK. Our dedicated and highly trained team aim to achieve consistently excellent results. For us it's more than just treating patients, it's about looking after people.
Important to note
The treatment described on this page may be adapted to meet your individual needs, so it's important to follow your healthcare professional's advice and raise any questions that you may have with them.
What is back surgery?
Different surgical procedures to remove or repair worn or damaged bones (vertebrae) or discs in your spine. Back surgery may also be used to relieve pain due to pressure on nerves (sciatica).
The type of surgery recommended depends on the cause of your back pain.
Causes of back pain
A common cause of back pain and sciatica is a slipped disc (herniated disc), where a spinal disc presses down on a nerve.
Back pain can also be caused by spinal stenosis, narrowing of the spaces in your spine, which puts pressure on a nerve, or cauda equina syndrome, a rare and severe form of spinal stenosis. Back surgery may be used after a spinal injury, a fracture due to osteoarthritis or to repair a displaced bone in your back (spondylolisthesis).
Cancer can also cause back pain needing surgery. This is called metastatic spinal cord compression, where cancer from one part of your body has spread into the spine and the mass of cells presses on the spinal nerves.
Back surgery can relieve back pain and aims to let you move more freely without pain. Surgery can also help you become more active, improve your mood, reduce your need for pain medication and may get you back to work if you’ve had to take time off. But for many people, it may not be necessary. Your doctor will usually recommend it only after you’ve had back pain for some time and have tried other treatments that haven’t worked for you.
Non-surgical treatments
These treatments include:
- Gentle exercise
- Painkillers
- Physiotherapy
- Psychological therapy
- Spinal injection therapy
Your doctor will assess your symptoms and will probably recommend an X-ray, a CT scan or an MRI scan. Our fast diagnostic service means you won’t have to wait long to find out if back surgery is right for you. At this appointment, your consultant will discuss which back pain treatment would be best for you and your lifestyle, so it’s a good time to talk about what you want.
Find your nearest Spire hospital
Almost all our hospitals offer private back surgery and have teams of orthopaedic (bone and muscle) and spinal surgeons who specialise in back pain treatment.

Events
Free mini consult with Dr Khafaga, Pain Management Consultant
Book a free mini consult with Mr Khafaga, to discuss your pain problems, explore different procedure and discuss your suitability
Learn more
Free knee pain information evening, with Orthopaedic Surgeon Mr Ganapathi
Join our free information evening, understand your knee pain, treatment options and see the ROSA knee robot in action!
Learn more
Free patient information evening for knee pain with Mr George Tselentakis
Join Consultant Orthopaedic Surgeon, Mr George Tselentakis for an evening talk.
Learn more
How back surgery works
There are many different types of back surgery and your consultant will recommend the one that will be best for you, depending on your condition. In some cases, more than one type of surgery will be performed in the same operation.
Types of back surgery
The most frequently used operations include:
Spinal (or lumbar) decompression surgery
Lumbar decompression surgery is used to treat spinal stenosis, cauda equina syndrome, slipped disc, metastatic spinal cord compression or a spinal tumour, and spinal injury. The main types are discectomy, laminectomy and spinal fusion.
Discectomy
A discectomy means the surgical removal of a whole or part of a spinal disc.
A disc is a fluid-filled cushion of tissue that sits between each vertebra and acts as a shock absorber. If it's damaged, fluid can leak out and put pressure on your spinal cord and surrounding nerves — this is a slipped disc and is a common reason for having a discectomy.
During the procedure, your surgeon will make a small cut over the affected area of your spine and remove any parts of the damaged disc that are putting pressure on your nerves. Most of the disc will be intact and it will still be functional.
There are two types of discectomy:
- Microdiscectomy — a minimally invasive technique where your surgeon inserts a microscopic camera to see the damaged disc and can perform the procedure via a small cut in your back
- Open discectomy — your surgeon accesses the damaged disc through a cut in your back or neck
Laminectomy
Your surgeon makes a cut into your back over the affected vertebrae and pushes aside the muscles as needed. They then remove the back part of one or more of your vertebrae, called the lamina, to relieve pressure on the spinal cord. This pressure is often a result of bony overgrowths in the spinal canal, which narrows the space in your spinal cord. It commonly occurs as you age.
The size of the cut made into your back will depend on the condition causing your back pain and the size of your body. In some cases, smaller cuts can be made and the procedure's performed using a special surgical microscope.
Your doctor may recommend laminectomy if you have spinal stenosis, where the spinal canal is narrowed through wear and tear, or if previous treatments for your back pain, such as medication and physiotherapy have failed and your symptoms are worsening. Laminectomy is also recommended if you find standing or walking difficult, or if you're experiencing a loss of control of your bladder or bowel.
Spinal fusion
There are three different ways your surgeon can approach this procedure. They can access your spine by making a cut into the front of your body, your side or your back. They will take a piece of bone from elsewhere in your body (usually your hip) to insert between two vertebrae to strengthen them and prevent painful movement. Alternatively, they may use a bone graft, which can be made from demineralised bone matrices (DBMs), bone morphogenetic proteins (BMPs) and synthetic bones.
You may have this surgery after a break or fracture, to help fix scoliosis, or if one of your vertebrae is displaced and is causing pain (spondylolisthesis).
Vertebroplasty or kyphoplasty
Both are similar types of procedures where bone cement is injected into the spine to repair the damage, often caused by osteoporosis. In kyphoplasty, a small balloon is inserted into the affected area and expanded to make space for the cement.
Foraminotomy
A procedure to relieve pressure and pain caused by vertebrae compressing on a nerve where it exits the spinal cord. Your surgeon will make a cut in your back and remove part of your vertebrae to open up space where the nerve exits the spinal cord.
Interlaminar implant
In this procedure, a device is inserted between two vertebrae to ease pressure on your spinal nerves.
Disc replacement
This is where a damaged disc is replaced with an artificial one. The damaged disc can be partially or fully removed. The new disc is designed to act in the same way as a healthy disc, allowing pain-free movement between your vertebrae.
Your consultant will discuss your options and recommend a treatment tailored to your diagnosis.
Advances in surgery
To find out more about recent advances and how back surgery is performed at your local Spire Healthcare hospital, use the hospital search tool above.
Preparing for back surgery
It’s important for you to be as fit as possible before your surgery as it will help you with your recovery and reduce your risk of any complications. Once you've agreed with your consultant that you'll be having back surgery, you should eat a healthy and balanced diet, exercise regularly and stop smoking.
You'll be asked to sign a consent form once you’ve decided to proceed with the surgery. You may also be asked to attend a pre-operative appointment to check that you’re fit for surgery. Here, you may undergo some blood tests and have an X-ray or MRI scan of your spine. During this assessment, you can also ask any questions and discuss your concerns about your surgery.
Your consultant will also advise if you should wear compression stockings and/or have an anti-clotting injection to prevent blood clots from forming after the procedure. You'll also be given instructions to follow on the day of your procedure, which may include washing with antibacterial soap and what to wear and bring with you.
You’ll have to stop eating for six hours before your back surgery, but you can drink clear fluids until two hours before. You’ll also need to arrange for a family member or friend to come and pick you up – travelling home on public transport is not advised.
Back (spinal fusion) surgery
Watch how back surgery takes place
View transcript of this video
This animation explains what happens during spinal fusion surgery.
The type of back surgery your surgeon may recommend will depend on the type of back problem you experience, such as sciatica, degenerative disc disease or spinal stenosis.
Surgery is usually only considered if non-surgical treatments haven’t worked and symptoms are affecting your quality of life.
The lumbar spine consists of five vertebrae, often referred to as L1 to L5. The lumbar vertebrae are the largest and carry most of the body’s weight, allowing for large movements.
Spinal fusion surgery is a procedure where two or more vertebrae are joined together with a section of bone in the space between them. This helps to prevent friction between two adjacent vertebrae, reduces the risk of further compression of the nearby nerve and elevates pain. The procedure is performed under general anaesthetic.
Once the surgeon has gained access to the spinal canal, the bone is clipped away as required and the disc is then removed.
A bone graft is used to fill the space created and fuses the two vertebrae together. Commonly, the patient's own bone is used, which is taken from the pelvic iliac crest – this is called an autograft.
A system of screws and rods is used to help keep your spine still while the bones are fusing together. They are placed on both sides of the vertebrae, above and below the disc space. These screws then act as firm anchor points to which rods can be connected. Over time, the bone graft grows and fuses to the spine.
The whole operation will take an hour, sometimes longer, depending on the complexity of the procedure. Any severe back pain you felt before your back surgery should now go away and you should be able to move about more easily.
Your doctor will discuss how to enjoy your usual activities safely and may advise against some activities like heavy lifting until you’ve fully recovered. Physiotherapy is also recommended to help your recovery.
For more information contact your local Spire hospital or visit the Spire Healthcare website.
What to expect during spine surgery
Who will be involved?
Your back surgery will be performed by an orthopaedic or neurological surgeon, but you’ll also be seen by an anaesthetist to administer anaesthetic during the operation. After your surgery, a physiotherapist will take you through some exercises you can perform at home.
How long does back surgery take?
Your operation will take at least an hour but may take much longer if you need a more complex procedure.
Anaesthetic
You’ll have a general anaesthetic, so you’ll be asleep and won’t feel anything during your operation.
Pain after back surgery
As with most operations, you’re likely to feel some discomfort afterwards, which may last days or weeks. You’ll be given painkillers and we can help you manage any pain as you recover. The good news is the severe back pain you felt before your back surgery should go away or improve, so you should be your active self again in a few months.
Your hospital stay
The average hospital stay is one to four days.
Q & A
Alwyn Jones, Consultant Orthopaedic Surgeon
Talking about back surgery
View transcript of this video
Is all back surgery the same?
Back surgery can vary between taking a disc out, to injections for different types of pain, to more major surgery. It depends on the underlying condition.
What is a spinal disc?
A disc is the body shock absorber for the spine. It sits between two vertebrae. It normally has two parts to it, the outer hard shell called the annulus, and the inner part which is the nucleus and more of a jelly-like material.
Why do these discs slip?
As we get older, our discs dry and they become more like crab meat. With regards to a disc slipping, the outer wall becomes weak and you’ll often get a crack or gap in the outer wall and then the inner nucleus will herniate (leak) out. Sometimes after major traffic accidents we see discs that are injured, but predominantly these discs become injured due to wear and tear and degenerative changes.
Will a slipped disc always cause pain?
Sometimes it can cause no trouble, apart from back pain, but on occasion it can hit or get close to the nerve and cause pain down the leg, like sciatica. If this occurs in the neck, it can cause arm pain.
How successful is back surgery?
With regards to back surgery for a herniated disc and sciatica surgery, normally 80 to 90% of people are better. The chances of making someone worse is probably in the vicinity of 5%, if they get a complication.
How long will it take me to recover from back surgery?
Normally the recovery time is dependent on your pre-operative activities. Most people are good by three months, but some people can return to work anywhere between six to eight weeks.
Recovering from back surgery
Back surgery recovery time
How quickly you recover from your surgery depends on how fit you were before and on the type of operation you have. After your surgery, you can expect to be in hospital recovering for one to four days.
Spinal (or lumbar) decompression surgery
It will usually take four to six weeks for you to return to your normal activities.
Discectomy recovery time
It will usually take six to eight weeks to return to your normal activities.
Laminectomy recovery time
It will usually take four to six weeks to return to your normal activities. If you have spinal fusion surgery alongside a laminectomy, your recovery may take longer.
Spinal fusion recovery time
It usually takes four to six weeks to return to desk-based work and around three months to return to more physical activities.
Vertebroplasty or kyphoplasty recovery time
You can usually return to your normal activities a day after your vertebroplasty or kyphoplasty. However, it is recommended that you avoid intense exercise and heavy lifting for several weeks.
Driving after surgery
You may be able to drive again as soon as two weeks after your surgery but you’ll need to check with your insurance policy first.
Returning to work
You’ll be able to return to desk-based work around four to six weeks after your surgery. However, if your job involves a lot of driving or heavy lifting, you may need to allow three months for recovery. You can also expect to return to your usual activities after two to three months.
Physiotherapy and ongoing treatment
Our expert aftercare team will encourage you to walk around the day after surgery and our physiotherapist will take you through a series of exercises to do at home. It’s important to carry on with these exercises to speed up your recovery, strengthen your muscles, reduce the risk of scarring around your nerves and avoid getting blood clots in your legs.
If you have stitches, they'll be removed after around 10 days. This may be done at the hospital you had your surgery at or one of our nurses will visit you at home.
Your lifestyle after treatment
Most people who have back surgery find that their symptoms improve, so they’re free from pain again and can move about easily.
Your dressing will need to be kept dry until your wound has been reviewed by a doctor, which may be up to seven days after the procedure. Once reviewed, you can wash as normal without the dressing.
You may find that in the days after your surgery staying in any position for too long causes discomfort. Changing positions regularly can help relieve this pain. Your back may also become stiff and painful overnight, so start your physiotherapy exercises before getting up.
Keeping to a routine, building up to activities gradually and having others to help you and to socialise with will all help with your physical and emotional recovery.
Your doctor will discuss how to enjoy your usual activities safely and may advise against some activities, such as heavy lifting or awkward twisting, until you’re fully recovered.
Treatment and recovery timeline
Your treatment and recovery timeline will depend on your particular circumstances, including the cause of your back pain, the severity of your condition, the specific procedure you have and your fitness before surgery.
However, as a general guide, you can expect to be in hospital for one to four days. After two to six weeks you can usually start driving again although you will need to check your car insurance policy.
After four to six weeks, you can return to desk-based work or work that is not too strenuous. However, if your job involves a lot of driving or heavy lifting, you may need to wait up to 12 weeks before returning to work.
You will usually be able to return to all of your usual activities in around two to three months.
Day 1
3 months
1-4 days
In hospital
2-6 weeks
Start driving again (check your insurance policy)
4-6 weeks
Return to work if your job isn’t too strenuous
Up to 12 weeks
Return to work if your job involves a lot of driving or heavy lifting
2-3 months
Return to your usual activities
-
1-4 days
In hospital
-
2-6 weeks
Start driving again (check your insurance policy)
-
4-6 weeks
Return to work if your job isn’t too strenuous
-
Up to 12 weeks
Return to work if your job involves a lot of driving or heavy lifting
-
2-3 months
Return to your usual activities
Risks and complications of back surgery
Most people have back surgery without complications but all surgery carries some risks, which your consultant will talk through with you before you go ahead.
If you have a vertebroplasty or kyphoplasty, you may develop a reaction to the bone cement used or it may leak inside your body.
During your surgery, certain tissues may become damaged such as your:
- Dura mater — the covering that sits over your spinal cord and nerves can be torn (dural tear), which may cause cerebrospinal fluid to leak into your body
- Spinal nerves or cord — your nerves could be stretched, bruised or damaged and this may lead to muscle weakness or bladder and bowel dysfunction
Other complications include:
- Bleeding or damage to blood vessels around your wound
- Blood clot in your legs — this is called deep vein thrombosis (DVT), this can also spread to an artery in the lung and cause a pulmonary embolism
- Facial sores — lying face down during your surgery can result in red sores on the forehead and chin or a puffed face
- Infection — this can occur around the site of surgery on your back; it is usually effectively treated with antibiotics
- No improvement in back pain or developing back pain symptoms again within a few years of surgery
- Paralysis — this is exceptionally rare
You should call a doctor right away if you experience any of the following symptoms after your back surgery:
- A sudden feeling of weakness or numbness which is not going away
- Fever
- Loss of bladder or bowel control
- Redness, swelling or oozing around the site of surgery
- Severe headache that is not improved with painkillers
- Severe pain unlike your normal symptoms
At Spire Healthcare hospitals, your safety is our top priority. We have high standards of quality control, equipment and cleanliness and a rigorous system of review and training for our medical teams.
Frequently asked questions
Is there anything I can do to help my recovery after back surgery?
Eating healthy, exercising regularly and not smoking will all help you recover from your back surgery quicker. Keeping to a routine, having others to help you with practical tasks, and building up to activities gradually will also help with your recovery.
Will I be able to play sports after my back surgery?
You may be able to return to most sports two or three months after your back surgery. It’s best to return to sports gradually and pace yourself while playing.
What are the different types of back surgery?
There are several different types of back surgery and the three most common are discectomy, laminectomy and spinal fusion. Additional types are vertebroplasty, kyphoplasty, foraminotomy, disc replacement and interlaminar implant.
How successful is lower back surgery?
The success rate for herniated disc and sciatica surgery is between 80 to 90%. As with all surgery, there are risks and complications that may occur, the chances of worsening your symptoms are around 5%.
How long does it take to recover from back surgery?
Everyone’s recovery will be different, but you should roughly allow two to three months to return to normal activities.
How does disc replacement differ from spinal fusion?
During a spinal fusion operation, your surgeon takes a piece of bone from elsewhere in your body and inserts it between two vertebrae to strengthen them. During disc replacement surgery, your surgeon will remove the damaged portion of the disc and replace it with an artificial disc.
What kind of doctor does back surgery?
Your back surgery will be performed by a surgeon of your choice and they will either be a neurological or orthopaedic surgeon.
Is endoscopic spine surgery safe?
Endoscopic spinal surgery is generally safe and in many cases may be safer than traditional open surgery. In cases where endoscopic surgery is not appropriate or open surgery is safer, your surgeon will explain the risks and benefits so you can make an informed decision.
Will a discectomy relieve back pain?
This will depend on the cause of your back pain. If you have a slipped disc, a discectomy may help relieve your pain.
Sources
https://www.bupa.co.uk/health-information/back-care/back-surgery
https://www.mayoclinic.org/tests-procedures/laminectomy/about/pac-20394533
https://orthoinfo.aaos.org/en/treatment/spinal-fusion/
https://www.nhs.uk/conditions/lumbar-decompression-surgery/recovery/
https://www.spine-health.com/treatment/spinal-fusion/postoperative-care-spinal-fusion-surgery
The treatment described on this page may be adapted to meet your individual needs, so it's important to follow your healthcare professional's advice and raise any questions that you may have with them.