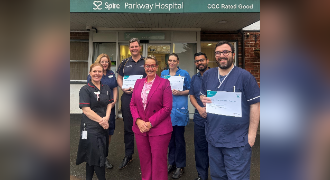
Grandfather of five regains his mobility after knee replacement surgery at Spire Parkway Hospital
27 June 2025
Gary Philpotts, a 65-year-old retired International Business Manager, turned full-time grandfather, received total knee replacement for both knees at Spire Parkway Hospital.