Knee replacement
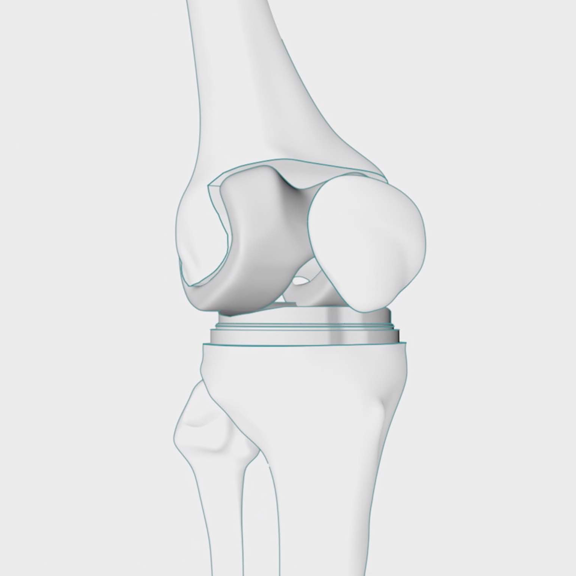
An artificial knee joint is used to replace the damaged joint.
We offer advanced surgical techniques and expert aftercare to replace painful damaged knee joints and help you get back to everyday activities.
Sometimes also called
- Patellofemoral replacement
- Partial knee replacement (PKR)
- Revision knee replacement
- Total knee replacement (TKR)
- Unicompartmental knee replacement
At a glance
-
Typical hospital stay
2–5 days -
Procedure duration
1–2 hours -
Type of anaesthetic
General, spinal or epidural -
Available to self-pay?
Yes -
Covered by health insurance?
Yes
Why Spire?
- Fast access to diagnostic tests and scans
- Consultants who are experts in their field
- Clear, inclusive pricing
- 98% of our patients are likely to recommend us to their family and friends
What is knee replacement surgery?
A knee replacement is a common operation to remove worn or damaged parts of your knee joint and replace them with an artificial joint, to help you move more easily and to reduce pain.
There are two main types of knee replacement — partial knee replacement and full knee replacement.
Knee pain is often caused by wear or damage, usually as a result of osteoarthritis but can also be caused by trauma or other conditions that damage the knee joint, such as:
- Avascular necrosis – death of the knee joint due to a lack of blood supply
- Bone dysplasia (unusual bone growth)
- Gout
- Haemophilia
- Knee deformity or injury
- Rheumatoid arthritis
Who needs knee replacement surgery?
You may need a knee replacement at any age, however, getting older increases your risk — those aged between 60 and 80 are most likely to need a knee replacement. Genetics, previous knee injury and lifestyle can also play a part in whether you need a knee replacement, so always seek medical advice if you have symptoms.
Your doctor may recommend knee replacement if:
- You find it difficult carrying out everyday tasks
- You have depression due to pain or reduced mobility
- Your mobility is reduced
- Your quality of life is impacted, including your sleeping
- You’re unable to work or socialise
Knee replacement surgery can relieve pain and help you become more active again. However, you must be healthy enough to undergo surgery.
Alternative treatments to knee replacement
Your doctor may suggest an alternative to knee replacement, although the results may not last as long. These treatments are often performed using arthroscopy — a type of keyhole surgery using a thin, flexible, telescopic instrument called an arthroscope.
Knee replacement alternatives include:
- Arthroscopic washout – flushing the knee joint with fluid using keyhole surgery, often performed with debridement (removal of loose bone or cartilage); this is less common than it used to be
- Ligament surgery to reconstruct damaged ligaments
- Microfracture – your surgeon makes small holes in your bones to stimulate cartilage growth
- Mosaicplasty – transferring healthy cartilage taken from the edge of your joint to the damaged area
- Osteotomy – the shin bone is cut and realigned to reduce the weight carried by the damaged part of your knee
Your doctor will usually only recommend surgery after you’ve tried other non-invasive alternatives to knee replacement without success. Other treatments include:
- Lifestyle changes
- Medications
- Physiotherapy
- Steroid injections
You’ll need to be examined by your orthopaedic surgeon. They will assess the range of movement of your knee, as well as its strength and stability.
You’ll also need an X-ray to show any wear or damage to your joint. Our fast diagnostics means you won’t have to wait long to find out whether knee replacement surgery is right for you. Your consultant will discuss what would be best for you and your lifestyle, so it’s a good time to talk about what you want. They will consider your:
- Activity level
- Age
- Knee size and shape
- Overall health
- Weight
As well as the potential benefits of reducing pain, increasing mobility and improving your quality of life, there are disadvantages of knee replacement surgery to consider:
- As with all major surgery, there are some risks of complications
- You’ll be less mobile for the first few weeks after the operation so you may need some help around the house and with errands
- Your new knee joint may eventually need revision surgery after about 20 years
- Your new joint won't be able to bend as far as a natural knee
Your consultant will take you through both the advantages and disadvantages of knee replacement surgery so you can make an informed decision.
Find your nearest Spire hospital
Almost all our hospitals offer private knee replacement surgery and have teams of orthopaedic (bone and muscle) surgeons who specialise in this procedure.

How knee replacement works
In a healthy knee joint
Your knee is a hinge joint formed where your thigh bone meets the shinbone of your lower leg. The ends of your bones and kneecap are covered in smooth cartilage — tissue that helps your bones glide easily across each other.
In an unhealthy knee joint
The cartilage is worn away, causing damage to the ends of your bones at the joint and making it painful and difficult to move.
Knee replacement surgery
Before your operation, you should try stay as active as possible and try strengthening muscles around your knee to help your recovery.
During the operation, your surgeon will position your knee in the bent position to better expose the joint. They will then make a 15-25cm incision below your knee and move your kneecap aside.
They will remove your damaged cartilage and the ends of your thigh bone and shinbone, and replace them with an artificial joint — the end of your thigh bone will be replaced with a metal shell and the end of your shinbone with a flat piece of plastic with a metal stem. Depending on the condition of your kneecap, they may also place a plastic button under the kneecap.
All of the artificial parts placed in your knee are together called the prosthesis. The prosthesis is measured to fit your joint beforehand. Once your prosthesis is in place, your surgeon will bend and rotate your knee to check it works properly.
The surgery is carried out under a general anaesthetic or a spinal or epidural anaesthetic where you’re awake but can’t feel anything below your waist.
There are two main kinds of knee replacements: total knee replacement surgery and partial knee replacement surgery.
Total knee replacement
Your surgeon will make an incision along the side of your knee to expose your kneecap and move it aside. They will remove the damaged ends of your thigh bone and shinbone and will replace both sides of your joint, and sometimes the back of your kneecap, with a precisely-measured prosthesis.
First, a dummy joint is placed so your surgeon can check that the joint works. Any adjustments are made and the bones cleaned before your final prosthesis is fitted.
Your surgeon replaces the end of your thigh bone with a curved piece of metal and your shinbone with a flat metal plate. A plastic spacer is positioned between the two metal parts to reduce friction as you bend your knee.
This prosthesis is fixed in place with cement and your wound cleaned and stitched up. Finally, a dressing is applied to protect your wound. In some cases, a splint is placed to keep your leg immobile, however, in most cases, it is recommended that you start moving your knee as soon as possible.
The procedure takes up to three hours.
Partial knee replacement
If you have less damage, your surgeon may only need to replace one side of your joint using a partial knee replacement.
Recovery will usually be faster and you may have greater improvement in your mobility and more natural movement than with a total knee replacement. One in four people with osteoarthritis is suitable for partial knee replacement.
For partial knee replacement, your surgeon may perform mini-incision surgery using smaller cuts and instruments to improve recovery time — this also reduces scarring. A blood transfusion after surgery is usually not needed.
As well as total and partial knee replacement, there are other procedures that may be suitable.
Kneecap replacement
Also called a patellofemoral replacement or patellofemoral joint arthroplasty, this is a less complex surgery than a knee replacement if only your kneecap is damaged. This is not usually suitable if you have osteoarthritis and the long-term outcomes are not yet clear.
Bi-lateral knee replacement
Also known double knee replacement surgery, the procedure involves replacing both knees at the same time. This may be suitable if you have osteoarthritis in both of your knees as it means you only need one surgery and one period of recovery. However, this surgery usually involves a longer recovery period and more support during your recovery than a single knee replacement.
Complex or revision knee replacement
If you have major bone loss, a deformity or ligament weakness, you might need a complex or revision knee replacement. The artificial joint has a longer stem that fixes into your bones and additional components that can give you more stability. Revision knee replacement surgery is also sometimes used if you need to have a knee replacement redone.
Advances in surgery
Exciting recent advances mean that surgeons can often operate using smaller incisions, so there’s less impact on your surrounding muscles and tendons and you’ll recover more quickly — this is called mini-incision surgery. Artificial joints (prostheses) can even be created using MRI scans and 3D printing to tailor the size and shape to your knee.
Some of our hospitals also use computer-assisted (image-guided) surgery to enable the surgeon to position the replacement more precisely. Some hospitals also use pre-programmable robotic arms to help fit your joint.
Knee replacement surgery
Watch how a knee replacement surgery takes place
View transcript of this video
This video explains what happens during a hip replacement surgery. A hip replacement is a common operation to remove worn or damaged parts of your hip joint and replace them with an artificial joint. It is often recommended if other treatments such as physiotherapy or steroid injections haven't helped reduce pain or improve mobility.
Your hip is the joint between the thigh bone or femur and the pelvis. The pelvis contains three bones called ilium, ischium, and pubis.
The hip joint is a ball-and-socket joint. The round head of the femur rests in a cavity, the acetabulum, that allows the rotation of the limb. The surface of these bones is coated with smooth, slippery cartilage also called articular cartilage which protects and cushions your bones allowing them to move easily next to each other.
When the cartilage is worn or damaged, the bones rub against each other causing pain and lack of mobility. Under an aesthetic, the surgeon will remove both the socket and the top of your thigh bone. The replacement components are the metal head and a plastic cup which are then inserted back into the socket of your pelvis.
A replacement ball on a stem will be inserted into your thigh bone. The ball is then placed into the socket putting your hip joint back together.
The surgery usually takes around 90 minutes. You should be able to leave the hospital after three to five days.
For the first weeks after the surgery, you'll need a walking aid such as crutches to help support you. Physiotherapy will help strengthen your muscles and ensure your new hip works at its best. For more information, contact your local Spire hospital or visit the Spire Healthcare website.
What to expect during knee replacement surgery?
Who will be involved?
As well as your chosen surgeon, your care team will include:
- A consultant radiologist — an expert in assessing images taken during scans (such as an X-ray or MRI scan)
- A physiotherapist — before and after surgery
- An anaesthetist to administer anaesthetic during the operation
A doctor is also available to see you if you have any medical issues or complications after surgery.
Preparing for your knee replacement operation
Your consultant or physiotherapist will recommend exercises you can do to strengthen the muscles around your knee before surgery to improve your recovery time.
It’s also a good idea to prepare your home for after your operation to make it easier for you to get around safely and more easily. Make sure you:
- Arrange to have crutches or a walking frame ready
- Have a stable bench or chair to use in your shower
- Have a stable chair with back support and a firm seat cushion
- Install:
a toilet seat raiser - safety handrails in your bath or shower
- safety handrails along your stairway
- Install:
- Make sure important items are easy to reach — arrange your living space so everything you need is on one floor to avoid having to climb stairs
- Remove anything you can trip over
Research what’s involved with a knee replacement surgery so you can ask your care team any questions and know what to expect on the day and during your recovery.
Before your operation, you’ll have a pre-operative assessment appointment with a nurse to check your general health before surgery and discuss any medications you’re currently taking that you may need to stop or adjust before surgery.
Most knee replacement surgery is carried out using general anaesthetic. Typically, you must not eat for about six hours or drink for two hours before general anaesthesia.
You will be told to avoid certain fluids (milk); instead, water or black tea or black coffee is usually recommended. You’ll also need to wear compression stockings during and after surgery to avoid blood clots in your leg while you’re immobile.
How long does knee replacement surgery take?
Usually between one and three hours, depending on whether you’re having a total knee replacement or a partial knee replacement.
Anaesthetic choices
Your consultant will help you decide what anaesthetic is best for you. You'll have either a general, spinal or epidural anaesthetic, so you’ll be fully unconscious or awake but unable to feel anything from the waist down. If you have the spinal or epidural options, you may have a sedative to help you feel more relaxed.
You may also receive a nerve block around your knee to numb it.
Before, during and after your surgery, you will be given antibiotics to prevent infection.
Pain after knee replacement
Everyone experiences pain differently and you’re likely to feel discomfort for some time afterwards. But don’t worry, you’ll be given painkillers after the operation and we can help you to manage any pain in the following days and weeks.
Your hospital stay
The average hospital stay is two to five days, with total knee replacements requiring longer than partial knee replacements.
Recovering from knee replacement surgery
Recovery can take several months and you’ll need to do knee replacement exercises and have physiotherapy regularly to improve your mobility.
Short term side effects
Immediately after your surgery, you may need to be given oxygen and/or a blood transfusion. Your wound may need to be drained and your dressings will need to be changed regularly. You will likely feel very tired.
You will have some pain in your knee after the operation so you’ll be given painkillers and you can continue to take over-the-counter painkillers when you’re home. You will need to use crutches or a walking frame at first.
Your knee, legs and feet may be swollen — you can try keeping your leg raised or using an ice pack in a tea towel for 20 minutes every three to four hours to help. Your care team will encourage you to move your foot and ankle to improve the blood flow to your leg muscles and help reduce swelling and prevent blood clots. They will also recommend breathing exercises and gradually increasing your activity level.
You’ll need someone to take you home after your operation and to help with errands around the house for the first few days as you regain some mobility. The stitches in your knee will need to be removed around 10-12 days after your operation or they’ll gradually disappear if they’re dissolvable stitches.
Physiotherapy and ongoing treatment
Soon after surgery, our physiotherapist will take you through a series of exercises designed to strengthen the muscles around your new knee and improve and optimise movement of the joint. It’s important you carry on doing them after you’ve left hospital. This will help speed up your recovery so you can enjoy normal activities again.
You will need to use a walking aid for around six weeks after your surgery.
Your lifestyle after treatment
Many people enjoy a full and active life after knee replacement surgery. You can take part in most low-impact sports, although your consultant will tell you if you need to wear a leg brace.
Our team will support you all the way to get the most from your surgery.
Looking after your new knee
You will need to use crutches or a walking frame after your knee replacement surgery but should gradually reduce the amount you need to use them.
Continue with the exercises prescribed by your physiotherapist to prevent stiffness but don’t force your knee into positions if it is not comfortable.
Make sure you wear supportive shoes when you are outside.
What not to do after a knee replacement
Make sure you do not:
- Kneel on your knee until your surgeon advises that you can
- Sit cross-legged for at least six weeks after your surgery
- Sleep with a pillow under your knee as this can cause a permanently bent knee
- Twist your knee
How long does a knee replacement last?
Most knee joint replacements last for 20 years or more. However, in one in 20 cases, further surgery will be needed in around 12 years.
Your prosthetic knee joint can wear out, particularly if you perform high-impact activities or are overweight.
Risks and complications of knee replacement surgery
Most people have knee replacement surgery without complications, but all surgery carries risks and your consultant will explain them to you before you go ahead.
Pain after knee replacement is a common short-term side effect — pain at night is particularly common. Swelling and weakness often also occur in the short term.
You’ll have some scarring, which will gradually fade with time.
Knee replacement surgery complications
Complications can include:
- A blood clot — this can occur in your:
- Leg — this is called deep vein thrombosis (DVT); symptoms include hard, hot, red or painful areas in your leg
- Lungs — this is called a pulmonary embolism (PE); it is rare but is a medical emergency; symptoms include chest pains and breathlessness
- A dislocated kneecap — in most cases, this can be repaired with surgery
- Abnormal bone growth — this may limit the movement of your knee and need further surgery to restore movement
- Excess scar tissue
- Failure of the artificial knee joint — this includes:
- Fracture — this may occur during or after surgery
- Infection of the knee joint — this is usually treated with antibiotics and further surgery
- Instability — this may need further surgery
- Joint stiffness
- Limited relief of pain or persistent knee pain
Other complications include:
- Blood vessel, ligament and/or nerve damage around your knee joint
- Numbness around the site of surgery
- Unexpected bleeding into your knee joint
Signs of serious complications
- Chest pain or breathlessness — these are signs of a PE (a blood clot in your lungs) and is a medical emergency
- Hard, hot, red or painful areas in your leg — these are signs of DVT (a blood clot in your leg)
Signs of infection after a knee replacement
- Chills
- Fever
- Fluid leaking from your wound
- Increasing pain, redness, swelling and tenderness in and around your knee
If your knee joint is infected, you will usually need antibiotics and further surgery to remove your prosthetic knee. After the infection has gone away, you will need to have another knee replacement surgery to install a new prosthetic knee.
Risks of general anaesthetic
Serious complications associated with general anaesthetic do occur, but they're extremely rare.
For most people, the benefits in terms of controlled unconsciousness and removal of pain are much greater than the disadvantages.
It’s estimated that serious complications result in approximately four deaths for every million anaesthetics given. The pre-operative assessment is carried out to limit the risk of any complications occurring.
Your risk of complications due to general anaesthetic increase with age and if you have underlying health conditions that affect your heart or lungs.
At Spire Healthcare hospitals, your safety is our top priority. We have high standards of quality control, equipment and cleanliness and an ongoing system of review and training for our medical teams.
Treatment and recovery timeline
Although everyone's different, in general, recovery from a total knee replacement will mean spending two to five days in hospital. On day one after your surgery, you should be able to stand using a walking aid. After a week you should be able to walk independently with crutches.
After four to six weeks, you may be able to drive but you will need to check with your car insurance company. After six weeks, you should be able to walk without crutches.
It can take anywhere from three months to one year before you are completely free from pain and swelling. After two years, your recovery will be complete as any scar tissue will have healed and your muscle strength restored through exercise.
Day 1
2 years
Day 1
You should be able to stand using a walking aid
2–5 days
You’ll be able to leave hospital
1 week
Able to walk independently with crutches
4–6 weeks
May be able to drive (check with your car insurance company)
6 weeks
Able to walk without crutches
3 months–1 year
Usually free from pain and swelling
2 years
Full recovery as scar tissue is healed and muscles restored by exercise
-
Day 1
You should be able to stand using a walking aid
-
2–5 days
You’ll be able to leave hospital
-
1 week
Able to walk independently with crutches
-
4–6 weeks
May be able to drive (check with your car insurance company)
-
6 weeks
Able to walk without crutches
-
3 months–1 year
Usually free from pain and swelling
-
2 years
Full recovery as scar tissue is healed and muscles restored by exercise
Frequently asked questions
How soon will I be up and about?
You’ll be helped out of bed to stand around 12 to 24 hours after your operation. You can then walk with a frame or crutches and should be able to do so independently after a week. If you’ve had keyhole surgery or are on an enhanced recovery programme, it may be sooner.
A physiotherapist will show you some exercises you can do to help strengthen your knee that you can start the day after surgery.
How long will it be before I feel normal?
It can take up to two years for your knee to recover, however, you should be able to resume normal daily activities within six weeks and any pain and swelling should settle within three months. Your leg may be swollen for up to a year.
When can I drive again?
You shouldn’t drive until it’s safe for you to do so – this means you should be able to comfortably make an emergency stop and be free from the sedative side effects of any painkillers. This is usually four to six weeks after your operation. Many insurance companies don’t insure you for a number of weeks after an operation, so make sure you check before you drive.
When can I go back to work?
Working can help your recovery by keeping you active. If you have a desk job, you can usually return to work around eight weeks after your operation, but it can be up to 12 weeks if you have a more physically active job.
When can I do housework?
You should be able to get back to most daily activities including light chores after six weeks. Avoid standing for too long to avoid ankle swelling and don’t stretch or bend down. You should avoid any heavy lifting or strenuous activity for three months after your operation.
How will it affect my sex life?
There’s no set time when it’s safe to have sex. You should treat it like any other physical activity during your recovery and gradually build up to it and only if it feels comfortable. Make sure you follow your physiotherapists advice about what movements to avoid.
Will I have to go back to the hospital?
You’ll return to hospital a few weeks after your operation for a follow-up appointment to check your recovery progress.
Will I need another new knee?
For most people, their new knee lasts around 20 years or even longer for total knee replacement. Partial knee replacements tend to need to be replaced sooner – after around 10 years. The chances of needing a repeat operation is higher if you’re overweight, you run, play vigorous sports or you conduct heavy manual work.
Are there any sports or activities I shouldn't do after my knee replacement?
You should gradually build up any activity, and should be able to manage walking or swimming around six to eight weeks after surgery, depending how fit you were before surgery. You should avoid high impact sports such as running, contact sports or weight lifting. Your consultant or physiotherapist will be able to advise which sports you can do, they may recommend avoiding tennis, squash and skiing, but cycling, dancing and golf may be fine.
How can I make my recovery easier?
Preparing for your surgery by being as fit as possible and strengthening your knee muscles will help improve your recovery time. Before your operation, it’s also a good idea to prepare your home to make it easier for you to get around safely and more easily. Remove anything you can trip over and make sure important items are easy to reach.
For the first few days or weeks at home, you may need someone to help you with errands and household chores.
When can I fly after knee replacement surgery?
Speak to your consultant or GP before flying to find out what’s right for you. It’s important to note that your chance of deep vein thrombosis (DVT) increases if you fly after recent surgery.
Airlines have their own regulations about passengers flying after surgery, so make sure you check beforehand.
What are knee implants made from?
Knee implants are made from high-grade plastics, polymers and metal alloys.
What kind of metal is used in knee replacements
There are several different metals commonly used in knee replacements, specifically cobalt-chromium, nickel, titanium and zirconium.
How much walking can I do after a knee replacement?
In the first one to three weeks after your surgery, you may only be able to stand and/or walk for around 10 minutes. As your recovery progresses, you will be able to walk further and with less assistance.
After six weeks, you may be able to walk a few hundred metres without a walking aid. It is important to gradually increase your activity level and walking is a good way to do this. However, listen to your body; if you are feeling overly tired or in pain, have a rest.
Can I run after a knee replacement?
It is best to avoid high-impact activities after a knee replacement and this includes running. It is still important to stay active, so you can try low-impact activities, such as cycling, dancing and swimming.
Can both knees be replaced at the same time?
Yes, both knees can be replaced at the same time. This may be recommended if you have osteoarthritis in both knees. However, the surgery and recovery time are longer — you will also need more support during your recovery.
Can you have a knee replacement if you are overweight?
Yes, you can have a knee replacement if you are overweight. However, being overweight puts you at greater risk of certain complications during and after surgery. Your doctor will discuss the benefits and risks of knee replacement surgery in your particular case with you so you can make an informed decision.
The treatment described on this page may be adapted to meet your individual needs, so it's important to follow your healthcare professional's advice and raise any questions that you may have with them.
Get in touch
Sources
http://www.boa.ac.uk/patient-information/expectations-of-an-orthopaedic-patient-preferring-private-treatment/
http://www.boa.ac.uk/patient-information/expectations-elective-orthopaedic-patients-revised-may-2014/
https://www.mayoclinic.org/tests-procedures/knee-replacement/about/pac-20385276
https://www.medicinenet.com/total_knee_replacement/article.htm
https://www.healthline.com/health/total-knee-replacement-surgery
https://www.nhs.uk/conditions/knee-replacement/
https://www.nhs.uk/conditions/knee-replacement/what-happens/
https://www.nhs.uk/conditions/knee-replacement/risks/
https://www.nhs.uk/conditions/knee-replacement/recovery/
https://www.health.harvard.edu/pain/4-types-of-knee-implants
https://www.arthritisresearchuk.org/arthritis-information/surgery/knee-replacement.aspx
https://www.versusarthritis.org/about-arthritis/treatments/surgery/knee-replacement-surgery/
https://www.nice.org.uk/guidance/cg177/chapter/1-Recommendations#diagnosis-2
https://www.nice.org.uk/guidance/qs87/chapter/Quality-statements
https://www.nice.org.uk/guidance/qs87/chapter/Quality-statement-1-Diagnosis