Sleep apnoea tests are used to help determine the levels and the severity of the airway blockages that you may have.
Why you might need it
Obstructive sleep apnoea (OSA) is defined as the cessation of airflow during sleep preventing air from entering the lungs caused by an obstruction. When you experience an episode of apnoea during sleep your brain automatically wakes you up, usually with a very loud snore or snort. In order to breathe again. people with sleep apnoea can experience these wakening episodes many times during the night and consequently may feel very sleepy during the day.
Sleep apnoea tests are used to help determine the levels and the severity of the airway blockages that you may have. The results can then be used to help determine what treatments may be effective for you.
How much does Sleep apnoea test cost at Spire Dunedin Hospital
We can't display a fee for this procedure just now. Please contact us for a quote.
Who will do it?
Our patients are at the heart of what we do and we want you to be in control of your care. To us, that means you can choose the consultant you want to see, and when you want. They'll be with you every step of the way.
All of our consultants are of the highest calibre and benefit from working in our modern, well-equipped hospitals.
Our consultants have high standards to meet, often holding specialist NHS posts and delivering expertise in complex sub-specialty surgeries. Many of our consultants have international reputations for their research in their specialised field.
Before your treatment
You will have a formal consultation with a healthcare professional. During this time you will be able to explain your medical history, symptoms and raise any concerns that you might have.
We will also discuss with you whether any further diagnostic tests, such as scans or blood tests, are needed. Any additional costs will be discussed before further tests are carried out.
Preparing for your treatment
We've tried to make your experience with us as easy and relaxed as possible.
For more information on visiting hours, our food, what to pack if you're staying with us, parking and all those other important practicalities, please visit our patient information pages.
Our dedicated team will also give you tailored advice to follow in the run up to your visit.
The procedure
Depending on your needs and your consultant, there are a variety of sleep apnoea tests.
Apneagraph
Apneagraph uses a pressure monitoring system to record breathing patterns and oxygen saturation levels as you sleep to identify if you have sleep apnoea and also the location of the obstruction that is causing it. This helps us to identify the treatments that will give you the greatest chance of successfully treating the causes of your snoring.
To set up the Apneagraph, a small tube containing sensors is placed through the nose and into the throat (the oesophagus). The other end of the tube is connected to the Apneagraph recorder that collects the information as you sleep. Additionally a small device will be taped to your index finger to measure pulse rate and oxygen saturation levels. It takes approximately 30 minutes to set up the Apneagraph and you will need to wear a loose fitting t-shirt for your appointment, or something you are comfortable sleeping in.
Once the Apneagraph is set up, you can go home with the Apneagraph sensors in place and a small chest belt which houses the data recorder. All equipment will be positioned so that you can continue your life as normal, including eating and drinking that evening. An appointment will be made for you to come back the following morning to have the Apneagraph recorder and sensors removed.
Why choose Spire?
We are committed to delivering excellent individual care and customer service across our network of hospitals, clinics and specialist care centres around the UK. Our dedicated and highly trained team aim to achieve consistently excellent results. For us it's more than just treating patients, it's about looking after people.
Important to note
The treatment described on this page may be adapted to meet your individual needs, so it's important to follow your healthcare professional's advice and raise any questions that you may have with them.
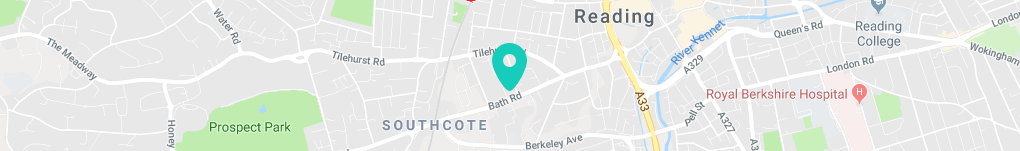
How to get to us
A 10-minute taxi ride from Reading railway station, we provide medical care to patients in Berkshire and the Thames Valley.
Spire Dunedin Hospital,
Bath Road
Reading
RG1 6NS
Get in touch
Important information about COVID-19 tests
COVID-19 testing or antibody tests are not available as a standalone service at Spire Dunedin Hospital.